Amber Diagnostics has an extensive selection of high quality refurbished and used medical imaging equipment for sale
Mobile Options
Mobile MRI, CT & PET/CT Scanners
Our top-tier MRI, CT, and PET/CT scanners are available to ensure seamless patient care and uninterrupted diagnostics.
For RentalFor Sale
Looking to sell your medical imaging equipment?
We buy used MRI, CT and PET/CT Scanners, C-Arms, Portable X-rays and other imaging equipment
how it Works
We Make it Easy
Amber Diagnostics has over 25 years of experience in the Medical Imaging Equipment industry and strives to provide high quality service to doctors and medical institutions.


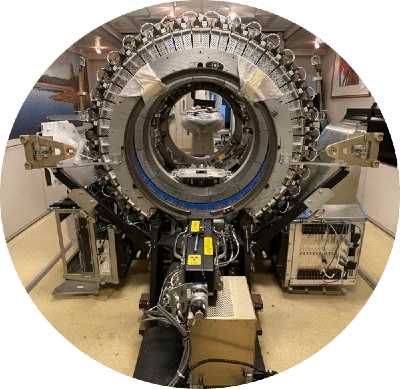
Refurbishment
We transform imaging equipment back into like-new condition so you can grow your business without going over budget.

Pack and Ship
We offer domestic and international shipping. Whether you need ocean or air export, we handle the process quickly and safely.
Site Preparation
We provide you with a blueprint that details from equipment location to wiring diagrams to ensure a smooth, planned-out process.

Installation
Our experienced service engineers and technicians will handle the installation safely while working around your facility’s schedule.
WE Have Many Options
Featured Equipment
Revolutionizing healthcare with used cutting-edge medical imaging equipment.
Let Us Help You
Grow Your Business
Download our helpful Buyer’s Guides that contain vital information regarding costs, parts, site planning, maintenance, and more. We also have a Return On Investment Calculator to help you determine how your investment is going to help your business.
Get Started
Request Pricing Today!
We’re here to help! Simply fill out the form to tell us a bit about your needs. We’ll contact you to set up a conversation so we can discuss how we can best meet your needs. Thank you for considering us!
Great support & services
Save time and energy
Peace of mind
Risk reduction